Title of the study:
“Assessment of the psychological and medical effects of the environmental factors color and light on patients and staff in the field of intensive care medicine”
Download evaluation_Helios_study_color_light_110319
Project partners:
Prof. Dr. Axel Buether
University of Wuppertal
Faculty of Design and Art
Gaussstrasse 20
42119 Wuppertal
Dr. Gabriele Wöbker
Chief Physician of the Clinic for Intensive Care Medicine
HELIOS University Hospital Wuppertal
Witten/Herdecke University
Location and scope of the study:
HELIOS University Hospital Wuppertal – Clinic for Intensive Care Medicine
A) Surgical Intensive Care Unit House 2, 8 patient rooms, 15 beds
B) Conservative (internal medicine/neurology) intensive care unit, building 5, 10 patient rooms, 20 beds
Period of the investigation:
24 months (2017/18)
Research questions:
- What influence does the color and lighting design of intensive care units have on the well-being and state of health of patients?
- What influence does the color and lighting design of intensive care units have on the work motivation, attitude and well-being of medical and nursing staff?
- What influence does the color and lighting design of intensive care units have on medication consumption?
Summary of the results:
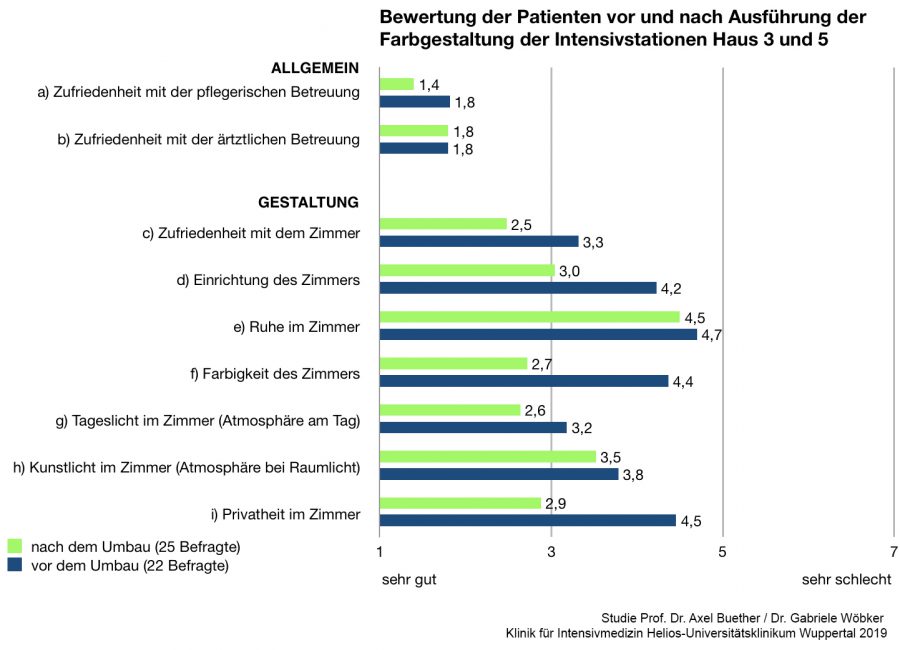
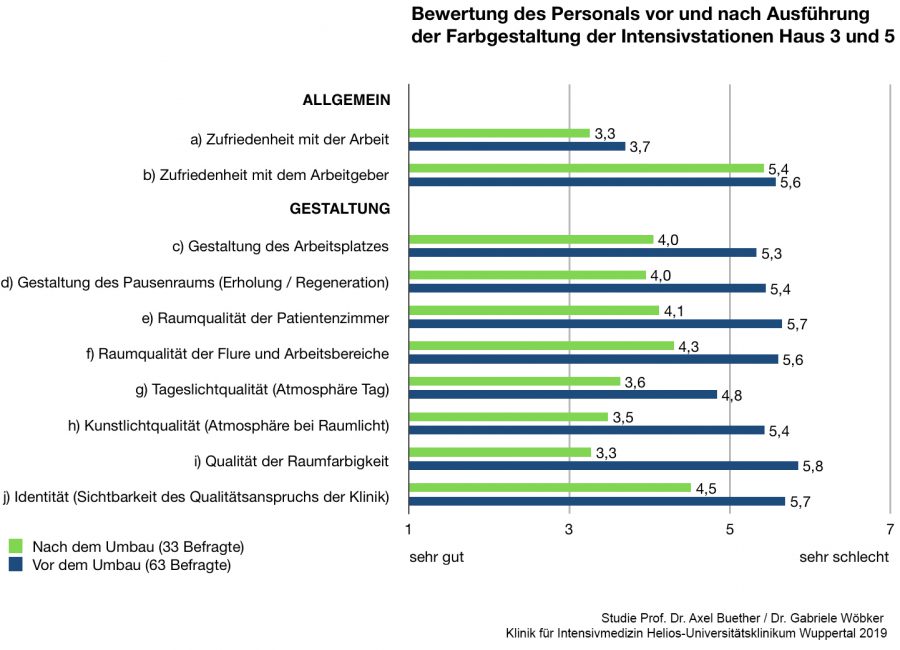
The effects of color and lighting design identified in qualitative and quantitative research are significant for both patients and staff. The patient surveys and the staff interviews before and after the renovation measures carried out prove the effectiveness of the psychological environmental factors of color and light on people’s well-being and satisfaction.
The perception of design factors increased by an average of 32.3% among patients and by as much as 40.8% among staff. Patients showed the greatest increase in their assessment of the color design (62.7%), closely followed by the feeling of privacy, which improved by 55.2%.
In terms of personnel, the largest increase of 75.6% was also recorded in color design, followed by the noticeable improvement in artificial lighting quality of 54.3%. This factor is all the more remarkable as new luminaires were not installed for cost reasons. The existing neon light sources were replaced with LED light sources with a color rendering index of 90, which makes the room colors appear relatively natural. The color temperature of the light in the patient rooms and staff lounges was kept warm white (3,000 K). In the corridors and functional rooms, however, with cool white or daylight white (4,000K). The contrast creates a “change of atmosphere that makes the lounges feel noticeably more homely, warmer and more secure. Perceptions such as deceleration and tranquillity were also described.
The effects of the spatial factors of color and light extend not only to the perception of architectural space, but also to the perception of care. The spatial impression of the common rooms and patient rooms, described by those affected as a “feel-good atmosphere”, ensures more effective care. The patients’ assessment of the care measures increased by 28% after the renovation. These indirect effects were also observed among staff, where job satisfaction rose by an average of 12%.
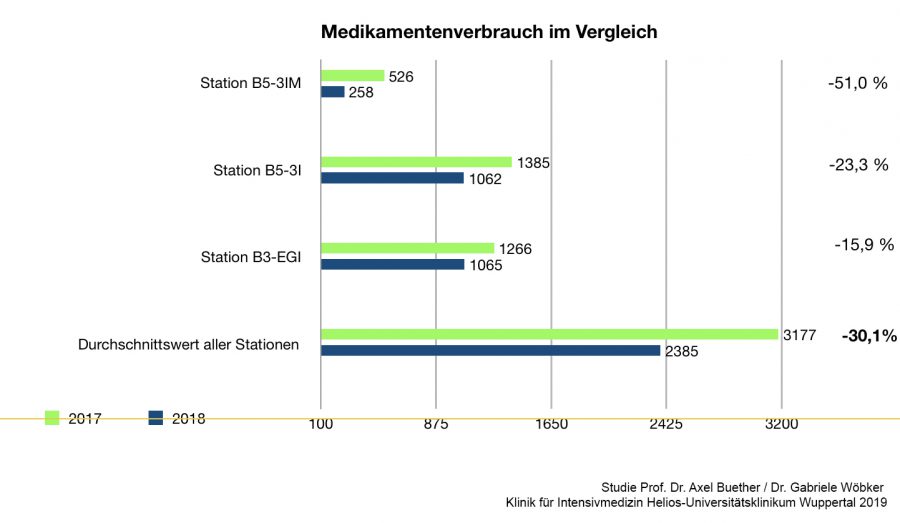
The consumption of medication has been significantly reduced. No significant changes were observed for benzodiazepines. There were significant changes in the acute neuroleptics (haloperidol, risperidone, chlorprothixene, etc.). In the same period, consumption fell by an average of 30.1%.
Occasion and objectives of the study:
This study was prompted by the current scientific debate in the field of intensive care medicine on the negative effects of prolonged delirium on patient morbidity and mortality. In addition to treatment with drugs, the search is now increasingly on for other factors that can promote the well-being and recovery of patients and prevent delirium. In this context, the focus is also shifting to the perception of architectural space, in particular the atmospheric effects of clinical environments. To date, there have only been a few studies worldwide that prove the influence of architectural space on people’s well-being and state of health. The research gap applies to the entire field of healthcare buildings. This is particularly problematic in the field of intensive care medicine, as the clinical environment can promote negative feelings such as anxiety, panic, disorientation, loneliness and depression. These effects can endanger the life and health of patients. In this context, the effects of architectural space on the well-being and job satisfaction of medical and nursing staff must also be considered.
Framework of the study:
The opportunity for this study arose on the occasion of upcoming renovation work on the B3-EGI, B5-3I and B5-3IMC wards of the Department of Intensive Care Medicine at HELIOS University Hospital Wuppertal. The renovation work was limited to repainting the walls, ceilings and doors and replacing all the light fittings. For cost reasons, it was not possible to renew the floors, furnishings and medical technology. The assessments of patients and staff were recorded both quantitatively before and after the renovation using questionnaires and qualitatively via interviews. In order to minimize distorting effects such as the impression of newness, the survey was only conducted 3 months after moving into the renovated rooms. Medication consumption was documented and evaluated in a representative comparison period of 9 months before and after the renovation. Evaluations of staff sickness levels and fluctuations in staff turnover will be carried out at a later date. The entire project was documented on film.
Delimitation:
In this study, we limited ourselves to examining the visual influencing factors of color and light. Other perceptual factors such as acoustics (speech, noises), smell (cleaning agents, disinfectants, materials) and taste (food, medication) were not taken into account in this study, but should be the subject of further research. The second focus of the study was on the effects of the architectural factors of color and light on the well-being and satisfaction of the medical and nursing staff, whose influence on the health of the patients should not be neglected. The acute shortage of skilled workers makes this question even more relevant. The two fundamental questions of this study concern not only the field of intensive care medicine, but the entire healthcare sector.
Sample room and view:
The sample room was equipped with biodynamic lighting, which enables day and night simulation and the adaptation of atmospheric conditions and counteracts the delirium state. The flooring was replaced with dissipative linoleum in a brown shade that blends harmoniously into the color concept. Feelings of safety, warmth and security were specifically strengthened. The renewed medical technology appears less threatening due to the hidden cabling. Turning the bed allows patients to look directly out of the window, which not only brings the sunlight into view, but also the colors of the sky and the treetops, which were previously limited to the ventilation elements in the ceiling. If the station is completely redesigned, significant increases in results can be expected, which should be investigated further.


Evaluation of the patient survey
Average design assessment and general satisfaction of patients on both wards in a before-and-after comparison (only some of the patients on both wards were surveyed, as only the responsive cases could be interviewed = the result is representative to a limited extent, but shows a clear trend; further studies are required)
GENERAL SATISFACTION: (Evaluation before/after)
a) Satisfaction with nursing care: improvement 28.6% (1.8/1.4 )
b) Satisfaction with medical care: Consistency 0% (1.8 /1.8)
SATISFACTION WITH THE ROOM (DESIGN): (Evaluation before/after)
c) Satisfaction with the room: improvement 32% (3.3/2.5)
d) Furnishing of the room: improvement 40% (4.2/3.0)
e) Quiet in the room: improvement 4.4% (4.7 /4.5)
f) Colorfulness of the room: improvement 62.7% (4.4/2.7)
g) Daylight in the room (atmosphere during the day): Improvement 23.1% (3.2/2.6)
h) Artificial light in the room (atmosphere with room light): Improvement 8.6% (3.8/3.5)
Privacy in the room (feeling of protection and security): Improvement 55.2% (4.5/2.9)
Average improvement in room factors: 32.3%
Evaluation of the staff survey
Average design assessment and general satisfaction of medical staff on both wards in a before-and-after comparison (almost all staff on both wards were surveyed = the result is representative)
GENERAL SATISFACTION: (Evaluation before/after)
a) Satisfaction with work (activity): Improvement 12% (3.7/3.3)
b) Satisfaction with the employer (care, appreciation): Improvement 3.7% (5.6/5.4)
SATISFACTION WITH THE WORKPLACE (DESIGN): (Evaluation before/after)
c) Workplace design: improvement 32.5% (5.3/4.0)
d) Design of the break room (recreation / regeneration): Improvement 35% (5.4/4.0)
e) Room quality of patient rooms: improvement 39% (5.7/4.1)
f) Room quality of corridors and work areas: Improvement 30.2% (5.6/4.3)
g) Daylight quality (atmosphere and lighting conditions during the day): Improvement 33.3% (4.8/3.6)
h) Artificial lighting quality (atmosphere with room lighting): Improvement 54.3% (5.4/3.5)
i) Quality of room color: improvement 75.6% (5.8/3.3)
j) Identity (visibility of the clinic’s quality standards): Improvement 26.7% (5.7/4.5)
Average improvement in room factors: 40.8%
Evaluation of medical data
Delirium in hospital:
In 2016 and 2017, the Intensive Care Medicine specialist group at HELIOS Kliniken GmbH made delirium a focus topic and established a Delirium Working Group, which is headed by Dr. Wöbker, Chief Physician at the Clinic for Intensive Care Medicine.
“Delirium is an acute disorder of cerebral function. While a third of internal medicine patients over the age of 70 develop delirium in hospital, the incidence in surgical patients is between 5.1% after minor surgery and 52.2% after major surgery, depending on the procedure performed. In intensive care patients, delirium occurs in 30-80% of cases – depending on the severity of the illness. Delirium is associated with an increase in mortality from 3.9% to 22.9%, a longer hospital stay of up to ten days and a poorer treatment outcome. In a study of intensive care patients, it was shown that the 1-year survival probability decreases by around 10 % with each day of delirium. Delirium leads to an increased need for post-inpatient care and around 25% of patients develop cognitive dysfunction after delirium, which is comparable to mild Alzheimer’s dementia.”
Question:
What effects do environmental factors such as color and light have on drug consumption in intensive care medicine?
Research setting:
The consumption of benzodiazepines and neuroleptics was measured over two time intervals of 9 months each before and after the color design.
Evaluation:
No significant changes were observed for benzodiazepines. There were significant changes in the neuroleptics. In the same period, consumption fell by an average of 30.1%. In the Intermediate Care Unit (IMC), where patients are admitted for up to 2 days, consumption fell by 51% in the same period. Consumption in the surgical intensive care unit (B3-EGI) fell by 15.9% in the same period. In the conservative (internal medicine/neurology) intensive care unit B5-3I (10 patient rooms, 20 beds), consumption fell by 23.3% in the same period.